
- Автоматизация
- Антропология
- Археология
- Архитектура
- Биология
- Ботаника
- Бухгалтерия
- Военная наука
- Генетика
- География
- Геология
- Демография
- Деревообработка
- Журналистика
- Зоология
- Изобретательство
- Информатика
- Искусство
- История
- Кинематография
- Компьютеризация
- Косметика
- Кулинария
- Культура
- Лексикология
- Лингвистика
- Литература
- Логика
- Маркетинг
- Математика
- Материаловедение
- Медицина
- Менеджмент
- Металлургия
- Метрология
- Механика
- Музыка
- Науковедение
- Образование
- Охрана Труда
- Педагогика
- Полиграфия
- Политология
- Право
- Предпринимательство
- Приборостроение
- Программирование
- Производство
- Промышленность
- Психология
- Радиосвязь
- Религия
- Риторика
- Социология
- Спорт
- Стандартизация
- Статистика
- Строительство
- Технологии
- Торговля
- Транспорт
- Фармакология
- Физика
- Физиология
- Философия
- Финансы
- Химия
- Хозяйство
- Черчение
- Экология
- Экономика
- Электроника
- Электротехника
- Энергетика
Docent Kamilova I.K.
Docent Kamilova I.K.
II.Tests for evaluation of endocrine status(functional diagnosis’ tests)
Endocrine status is assessed by such a functional diagnosis parameters as the cytologic pattern of a vaginal smear, the “pupil” symptom, “fern” symptom (arborization of cervical mucus), a viscosity and stretch ability of cervical mucus, and rectal (basal) temperature, as well as by findings of endometrial biopsy, hormonal levels in the blood plasma and urine and by hormone assays.
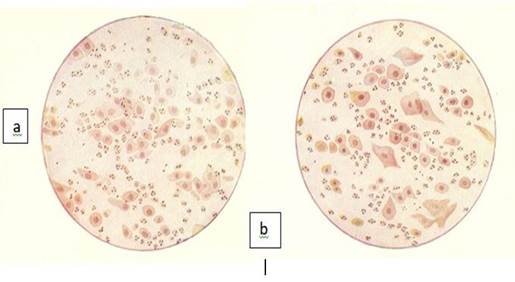
Cytologic pattern of a vaginal smear. To study the cytologic pattern of vaginal smears, the discharge from one of the lateral fornices is spread in a thin layer on a glass slide, air-dried, fixed in an alcohol-ether mixture, and then stained with hematoxylin-eosin. The effect of estrogens on the stratified squamous epithelium is expressed in epithelial cornification, degree of which is directly correlated with estrogen concentrations. The predominance in a smear of cornified cells testifies to a high content of estrogen (hyperestrogenism). When estrogen levels are moderate, the so-called intermediate cells are sloughed from the vaginal wall. In patients with low concentrations of estrogens (hypoestrogenism associated with ovarian hypofunction or menopause) basal cells from deeper layers are shed and prevail in a smear. (Fig 34)

Fig. 34.Types of epithelial cells of vagina.
Depending on the ratio between the types of epithelial cells, four types of vaginal smears are distinguished:
type I: a smear consists of basal cells (small round or oval in shape with a relatively large nucleus) and leucocytes. This type is typical of very pronounced estrogen deficiency. It is observed in postmenopausal women and in young women with ovarian hypofunction and amenorrhea;
type II: a smear contains basal and intermediate cells, with the predominance of basal cells and leucocytes. It occurs in considerable estrogen deficiency (ovarian hypofunction, post menopause);
type III: intermediate cells are the most predominant in a smear. It is a characteristic of moderate estrogen deficiency;
type IV: a smear is composed of cornified cells. It is observed in sufficient estrogen saturation. (Fig. 35 a,b,c,d)
Types III and IV are noted in normal menstrual cycle (depending on the phase of the cycle).
|
c – type III; d – type IV.
The cytologic pattern may also be quantitated, which involves the determination of the percentage ratio of surface cells with pyknotic nuclei to the total number of surface cells (caryopyknotic index, ripening index).
The KaryopyknoticIndex (KPI). The karyopyknotic index expresses the percentile relationship of superficial squamous cells with pyknotic nuclei to all mature squamous cells (with vesiculae nuclei). Usually, 200 to 400 consecutive cells in three or four different fields on the smear are evaluated. The smear is taken from the lateral fornix of the vagina as cells here respond to cyclical changes in hormone that occurs in the menstrual cycle. The KPI correlated significantly with the plasma estradiol. The peak of KI usually coincides with the time of ovulation.
Examples: KPI > 25% - in proliferative phase of endometrial cycle
KPI < 3-5% -very low, corre3spond to secretory phase
KPI : 50-85% - typical for day of ovulation
KPI > 10% in pregnancy – progesterone deficiency
The Eosinophilic Index (EI). The eosinophilic index expresses the percentile relationship of mature squamous cells with eosinophilic cytoplasm to all mature squamous cells, regardless of the status of the nucleus. In a normal menstruating woman, the peak of EI coincides with the peak of KI and may reach 50% to 75% at the time of ovulation.
The Maturation Index (MI) expresses the maturation of the squamous epithelium as a percentile relationship of parabasal cells to intermediate cells to superficial cells. MI is determined by the count of 100-200 cells in 5-8- eye shots (field of vision), and expressed in per cents. MI is designated as a formula, where the amount of basal cells is written down on the left, in the middle – intermediate, on the right – cornified cells. 0 designates the absence of some types of cells.
In a normal menstruating woman at the time of ovulation, an MI of 0:35:65 would indicate that the smear contained no parabasal cells, 35% of intermediate cells, and 65% of superficial cells.
MI Examples.
MI = 100/0/0: there are only basal cells in the smear, no intermediate and cornified, means significant atrophy.
MI=70/30/0: there is 70% of basal and 30% of intermediate cells in the smear, no cornified, means moderate atrophy.
MI= 0/80/20: no basal cells in the smear, there is predominance of intermediate cells (80%), and about 20% of cornified cells, means moderate proliferation.
MI=0/20/80: no basal cells, there is about 20% of intermediate and 80% of cornified cells in the smear, means significant proliferation.
MI shows the functional activity of ovaries, it helps to determine the changes of ovarian function depending on hormonal therapy.
Cervical mucus reveals a number of rheologically related properties including viscosity, stretchability, flow elasticity or retraction, plasticity and tack. Rheology is the study of the flow and deformation of matter. In the case of the cervical mucus, however, this term is extended to include various biophysical properties and also some viscoelastic characteristics of molecular physics.
“Pupil” symptom. The “pupil” symptom consists in the following. In the follicular phase the cervical glands produce a mucous secretion, the largest amount of which is accumulated by the mid-cycle. The external os of the cervix is dilated by this secretion as a result and resembles a pupil, which can be seen during speculum examination. This symptom is observed from day 10 to day 17 of the cycle, being most pronounced on day 14-15. In women with estrogen deficiency this symptom is either weak or absent, whereas in patients with excessive estrogen production it may persist for longer time. The less degree of dilatation of external os due to accumulation of mucus is designated as +, moderate ++, maximal (0. 25-0. 3 cm) +++.
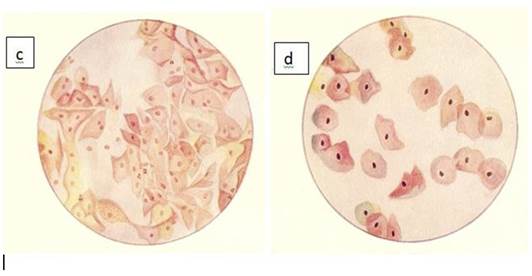
Crystallization of cervical mucus (syn.: “fern” symptom, arborization symptom). Of all the properties of mucus “crystallization”, i. e. arborization or fern phenomenon, is undoubtedly one of the most sensitive to changes in the level of sex hormones. Thus “ferning” is widely used for the detection of ovulation and for assessing corpus luteum function, in the early diagnosis of pregnancy and even of a threatened abortion, and in monitoring the induction of ovulation. The arborization is not specific to cervical mucus; it can be seen in other mucous secretions and in most body fluids as well. It occurs in all solutions containing proteins or other organic compounds and electrolytes, particularly sodium chloride. Although not specific in other body fluids, arborization in cervical mucus is distinctly dependent upon the action of estrogen and bears a close relationship to the two rheological properties described above, viscosity and spinnbarkeit. The extent of crystallization of the mucus bears a direct relationship to sperm receptivity.
The fern pattern appears during the early proliferative phase, usually at about the 5th or 6th day of the 28-day cycle increasing proportionally with the degree of estrogenic activity. It reaches a maximum at ovulation and 24-72 hours later it begins to be replaced by a cellular pattern characteristic of progestational activity. The fern pattern usually disappears completely by the 22nd day of the cycle. Pregnancy and the administration of progesterone both produce the same qualitative picture as seen in the luteal phase of the normal cycle. Maximal arborization is likely to be found at the time of maximal spinnbarkeit and will usually precede the shift in basal body temperature by 24-48 hours. The peaks of arborization and spinnbarkeit also coincide with maximal receptivity to sperm and greater sperm penetrability.
The test, easily performed in the office or clinic, is carried out as follows: after the cervix is exposed and gently swabbed clean, a sample of endocervical mucus is obtained with a dry sterile plastic cannula or glass pipet and is spread on a clean glass slide. If the secretion is spread too thinly or if blood is present, arborization does not occur, even when adequate estrogen levels exist. The slide is air-dried for at least 10 to 20 minutes (drying must be absolutely complete) and then is read under both low- and high-power magnification on the microscope. If true arborization with crystallization is present, it is indicative of a predominant estrogen effect, and the test is positive If a cellular pattern without crystallization and arborization is seen, the test is negative and indicates either little or no estrogen effect or, more commonly, suppression of estrogen activity by progesterone. As an indirect quantification of the extent and intensity of estrogen effect, the cervical ferning can be graded according to the branching of the ferning pattern upon crystallization: grade 1 for primary branching, grade 2 for secondary branching, grade 3 for tertiary branching, and grade 4 for quaternary branching, the maximum observable. (Fig.36).
|
|
|
|

Fig.36. Crystallization of cervical mucus (“fern” symptom)
a- on the 10th day of menstrual cycle; b- on the14th day of cycle;
c- on the15th day of cycle; d- on the 22nd day of menstrual cycle.
Diagnostic use. Ovulation and the production of progesterone by the corpus luteum normally result in a shift from the positive fern test characteristic of the preovulatory phase to a negative test typical of the latter half of the menstrual cycle. Therefore this simple office procedure can be employed as an index of ovulation and normal corpus luteum function. Because both low estrogen levels and chronic endocervicitis may lead to a continually negative test throughout the cycle, at least two tests must be done, one during each half of the cycle for a valid conclusion to be reached.
Stretchability of cervical mucus. Stretchability (syn.: spinnbarkeit) pertains to the capacity of liquid to be drawn into threads. This characteristic also varies in cervical mucus during the menstrual cycle. There is a gradual increase in spinnbarkeit from the end of menstruation until ovulation, when it is at its peak. Following ovulation little or no spinnbarkeit can be demonstrated. The German term 'spinnbarkeit' is more widely used than the English equivalent expression “fibrosity, thread ability or elasticity”. Although this rheological property is one of the easiest to measure objectively, it is also one of the least accurate, yet it has considerable application both diagnostically and therapeutically. Most investigators use the simple technique of drawing the mucus away from a slide with a cover slip and measuring the length of the mucus thread, which can also be determined by the length to which the mucus thread can be drawn when the jaws of forceps are opened. This phenomenon is attributable to the presence of the long molecules in the mucus and is probably dependent upon branching of molecular chains and other strong intermolecular forces. (Fig.37)
Stretchability gradually increases during the proliferative phase of the cycle reaching a maximum of 15-10 cm immediately before or coincident with the ovulatory phase and the thermal shift of the basal body temperature chart. As with the arborization phenomenon (see below), after ovulation there is a subsequent decrease in the spinnbarkeit, signifying the advent of a progesterone effect.
Its assessment is frequently used as an optimal time for intercourse or for artificial insemination. The evaluation of stretchability is also useful as a biological parameter of an estrogenic effect on the endocervical glands. It is also being used for detection of the fertile period.
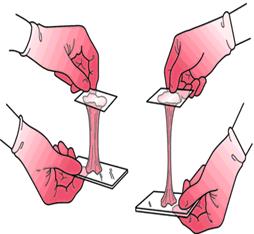
Fig.37. Stretchability of cervical mucus (spinnbarkeit).
Basal body (rectal) temperature (BBT). The basal body (rectal) temperature is measured in the morning before getting up. In the normal cycle the rectal temperature fluctuates throughout the cycle: in the follicular phase the basal body temperature is 36. 2 - 36. 7°C, in the luteal phase it increases by 0. 4-0. 5°C, declining again with the onset of menstruation. (Fig. 38).

Fig.38. Basal body temperature chart.
The basal body temperature fluctuations depend on the estrogen/progesterone ratio. Normally, the biphasic chart indicates the ovulation (ovulatory or biphasic menstrual cycle). In the absence of ovulation the temperature chart will be monotonous, monophasic (anovulatory menstrual cycle).
The presence of the ovulatory and luteal phases is confirmed by a histological examination of the endometrium, namely its secretory transformation. The curettage of the uterine cavity (scrapping of the endometrium) should be performed in the second half of the menstrual cycle. The absence or insufficiency of the secretory transformation of endometrium suggests luteal dysfunction.
The endocrine status of the patient is also evaluated by hormonal concentrations in the blood serum and urine. To specify the level of the impairment (hypothalamus, pituitary gland, ovaries, adrenal cortex) and the cause of endocrine lesion, various functional tests may be employed (progesterone, releasing hormones, LH, FSH, HCG, ACTH, synthetic progestins, glucocorticoids etc).
|
|
|
© helpiks.su При использовании или копировании материалов прямая ссылка на сайт обязательна.
|