
- Автоматизация
- Антропология
- Археология
- Архитектура
- Биология
- Ботаника
- Бухгалтерия
- Военная наука
- Генетика
- География
- Геология
- Демография
- Деревообработка
- Журналистика
- Зоология
- Изобретательство
- Информатика
- Искусство
- История
- Кинематография
- Компьютеризация
- Косметика
- Кулинария
- Культура
- Лексикология
- Лингвистика
- Литература
- Логика
- Маркетинг
- Математика
- Материаловедение
- Медицина
- Менеджмент
- Металлургия
- Метрология
- Механика
- Музыка
- Науковедение
- Образование
- Охрана Труда
- Педагогика
- Полиграфия
- Политология
- Право
- Предпринимательство
- Приборостроение
- Программирование
- Производство
- Промышленность
- Психология
- Радиосвязь
- Религия
- Риторика
- Социология
- Спорт
- Стандартизация
- Статистика
- Строительство
- Технологии
- Торговля
- Транспорт
- Фармакология
- Физика
- Физиология
- Философия
- Финансы
- Химия
- Хозяйство
- Черчение
- Экология
- Экономика
- Электроника
- Электротехника
- Энергетика
Laboratory Studies. Prehospital Care
Laboratory Studies

Laboratory tests are not helpful in detecting retinal detachment and are not warranted in the acute care of the patient. However, if the patient requires surgical intervention, it may be useful to have basic blood work (BMP, PT/PTT, INR, HbA1C). This is especially important in diabetics and those on systemic anti-coagulation.
 |
 |
Imaging Studies
Unless globe rupture, orbital/facial bone fractures or intraocular foreign bodies are suspected, imaging techniques, such as CT scans or MRIs, are not warranted to evaluate for retinal detachments.
In difficult cases, bedside ocular ultrasonography can facilitate prompt diagnosis of retinal detachment. Potential ultrasonographic mimics of retinal detachment (eg, posterior vitreous detachment [PVD] and vitreous hemorrhage [VH]) should be excluded.
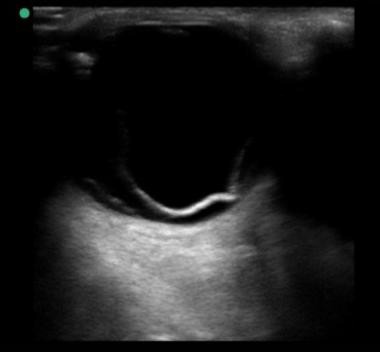 |
Sonogram of retinal detachment. Courtesy of Bruce Lo, MD.
 |
Treatment
Prehospital Care

When patients with retinal detachment or their family member contacts their physician, they should be advised to do the following:

 Keep the patient NPO (absolutely no solid foods or fluids) in anticipation of retinal surgery In cases of associated trauma, protect the globe with metallic eye shield
Keep the patient NPO (absolutely no solid foods or fluids) in anticipation of retinal surgery In cases of associated trauma, protect the globe with metallic eye shield
 Avoid any pressure on the globe and to limit activity to a minimum until further evaluation
Avoid any pressure on the globe and to limit activity to a minimum until further evaluation
 |
 |
Emergency Department Care
ED treatment of retinal detachment consists of evaluating the patient and treating any unstable vital signs, preparing the patient for possible emergency surgery. Please see the examination guidelines as stated above.
In difficult cases, bedside ocular ultrasonography can facilitate prompt diagnosis of retinal detachment. Potential ultrasonographic mimics of retinal detachment (eg, posterior vitreous detachment [PVD] and vitreous hemorrhage [VH]) should be excluded.
Patient follow up should be based upon macula status: Whenever a macula-on retinal detachment is suspected, a retina specialist should evaluate the patient within 24 hours.
All patients should be instructed to limit strenuous physical activity. Upon discharge from the ED, patients should be provided with the name and contact information for a retina specialist located close to their home.
There exists a multitude of techniques for treating retinal detachments, including scleral buckling, pars plana vitrectomy, and pneumatic retinopexy. The retinal detachment repair is usually done on an outpatient basis.
 |
 |
Consultations
Ideally, patients with retinal detachment should be quickly referred to a retina specialist. The timing of surgical intervention is typically based on the status of the macula.
 |
 |
Further Inpatient Care
Immediate ophthalmologic referral is mandatory for patients with retinal detachment.
 |
 |
Transfer
Emergent transfer to a facility with an available retina specialist is rarely indicated, as majority of cases can be evaluated within 24 hours. In some cases, transfer to a facility with an available ophthalmologist or retinal specialist is in the patient's best interest after initial ophthalmologic evaluation. Make these decisions in accordance with the patient's wishes and the direction of the ophthalmology consultant.
Contributor Information and Disclosures Author
Hemang K Pandya, MD Fellow in Vitreoretinal Disease and Surgery, Dean McGee Eye Institute, University of Oklahoma College of Medicine
Hemang K Pandya, MD is a member of the following medical societies: American Academy of Ophthalmology, American Society of Retina Specialists, Association for Research in Vision and Ophthalmology, Michigan State Medical Society, Michigan Society of Eye Physicians & Surgeons
Disclosure: Nothing to disclose. Coauthor(s)
Asheesh Tewari, MD Associate Professor, Division of Vitreoretinal Surgery, Department of Ophthalmology, Kresge Eye
Institute, Wayne State University School of Medicine
Asheesh Tewari, MD is a member of the following medical societies: American Academy of Ophthalmology, American Society of Retina Specialists, Association for Research in Vision and Ophthalmology, Michigan Society of Eye Physicians & Surgeons, Michigan State Medical Society
Disclosure: Serve(d) as a director, officer, partner, employee, advisor, consultant or trustee for: Bausch and Lomb; Dutch Ophthalmic< br/> Serve(d) as a speaker or a member of a speakers bureau for: Allergan.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape. Chief Editor
Bruce M Lo, MD, MBA, CPE, RDMS, FACEP, FAAEM, FACHE Medical Director, Department of Emergency Medicine, Sentara Norfolk General Hospital; Professor and Assistant Program Director, Core Academic Faculty, Department of Emergency Medicine, Eastern Virginia Medical School
Bruce M Lo, MD, MBA, CPE, RDMS, FACEP, FAAEM, FACHE is a member of the following medical societies: American Academy of Emergency Medicine, American Association for Physician Leadership, American College of Emergency Physicians, American College of Healthcare Executives, American Institute of Ultrasound in Medicine, Emergency Nurses Association, Medical Society of Virginia, Norfolk Academy of Medicine, Society for Academic Emergency Medicine
Disclosure: Nothing to disclose. Additional Contributors
Robert E O'Connor, MD, MPH Professor and Chair, Department of Emergency Medicine, University of Virginia Health System
Robert E O'Connor, MD, MPH is a member of the following medical societies: American Academy of Emergency Medicine, American College of Emergency Physicians, American Heart Association, American Medical Association, National Association of EMS Physicians, Society for Academic Emergency Medicine
Disclosure: Nothing to disclose. Acknowledgements
Gregory L Larkin, MD, MS, MSPH, FACEP Professor, Department of Emergency Medicine, Yale University School of Medicine
Gregory L Larkin MD, MD, MS, MSPH, FACEP is a member of the following medical societies: American College of Emergency Physicians, American Society for Bioethics and Humanities, Association for the Advancement of Automotive Medicine, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Douglas Lavenburg, MD Clinical Professor, Department of Emergency Medicine, Christiana Care Health Systems
Douglas Lavenburg, MD is a member of the following medical societies: American Society of Cataract and Refractive Surgery
Disclosure: Nothing to disclose.
References
1. Mattioli S, Curti S, De Fazio R, Mt Cooke R, Zanardi F, Bonfiglioli R, et al. Occupational lifting tasks and retinal detachment in non-myopics and myopics: extended analysis of a case-control study. Saf Health Work. 2012 Mar. 3(1): 52-7. [Medline]. [Full Text].
2. Haimann MH, Burton TC, Brown CK. Epidemiology of retinal detachment. Arch Ophthalmol. 1982 Feb. 100(2): 289-92. [Medline].
3. Subramanian ML, Topping TM. Controversies in the management of primary retinal detachments. Int Ophthalmol Clin. 2004 Fall. 44(4): 103-14. [Medline].
4. Bjerrum SS, Mikkelsen KL, La Cour M. Risk of Pseudophakic Retinal Detachment in 202? 226 Patients Using the Fellow Nonoperated Eye as Reference. Ophthalmology. 2013 Sep 8. [Medline].
5. McNamara D. Cataract surgery may up retinal detachment risk 4-fold. Medscape Medical News. September 13, 2013. Available at http: //www. medscape. com/viewarticle/811031. Accessed: September 24, 2013.
6. Lin H, Lema GM, Yoganathan P. PROGNOSTIC INDICATORS OF VISUAL ACUITY AFTER OPEN GLOBE INJURY AND RETINAL DETACHMENT REPAIR. Retina. 2015 Oct 14. [Medline].
|
|
|
© helpiks.su При использовании или копировании материалов прямая ссылка на сайт обязательна.
|