
- Автоматизация
- Антропология
- Археология
- Архитектура
- Биология
- Ботаника
- Бухгалтерия
- Военная наука
- Генетика
- География
- Геология
- Демография
- Деревообработка
- Журналистика
- Зоология
- Изобретательство
- Информатика
- Искусство
- История
- Кинематография
- Компьютеризация
- Косметика
- Кулинария
- Культура
- Лексикология
- Лингвистика
- Литература
- Логика
- Маркетинг
- Математика
- Материаловедение
- Медицина
- Менеджмент
- Металлургия
- Метрология
- Механика
- Музыка
- Науковедение
- Образование
- Охрана Труда
- Педагогика
- Полиграфия
- Политология
- Право
- Предпринимательство
- Приборостроение
- Программирование
- Производство
- Промышленность
- Психология
- Радиосвязь
- Религия
- Риторика
- Социология
- Спорт
- Стандартизация
- Статистика
- Строительство
- Технологии
- Торговля
- Транспорт
- Фармакология
- Физика
- Физиология
- Философия
- Финансы
- Химия
- Хозяйство
- Черчение
- Экология
- Экономика
- Электроника
- Электротехника
- Энергетика
ABSTRACT. ABSTRACT. INTRODUCTION
MINISTRY OF EDUCATION AND SCIENCE OF RUSSIAN FEDERATION
Federal State Autonomous Educational Institution of Higher Education
«V. I. VERNADSKY CRIMEAN FEDERAL UNIVERSITY»
Medical Academy named after S. I. Georgievsky.
ABSTRACT
SUBJECT : TYPES OF DIALYSIS: INDICATION, CONTRAINDICATIONS, COMPLICATIONS
STUDENT : Ranjith Kumar Mouleeshwaran
Faculty International Medical Faculty course 3rd course group La1-182(1)
PRACTICE PROGRAM : Procedural Medical Nurse Assistant.
PRACTICE PERIOD: from 27/06/2021 to 21/07/2021
ABSTRACT
Dialysis substitutes the natural work of the kidneys, so it is also known as renal replacement therapy (RRT). Healthy kidneys regulate the body’s levels of water and minerals and remove waste. The kidneys also secrete certain products that are important in metabolism, but dialysis cannot do this. People with failed or damaged kidneys may have difficulty eliminating waste and unwanted water from the blood. Dialysis is an artificial way of carrying out this process. Dialysis can carry out the function of the kidneys if the kidneys no longer work effectively. A healthy person’s kidneys filter around 120 to 150 quarts of blood each day. If the kidneys are not working correctly, waste builds up in the blood. Eventually, this can lead to coma and death. The cause might be a chronic, or long-term condition, or an acute problem, such as an injury or a short-term illness that affects the kidneys. Dialysis prevents the waste products in the blood from reaching hazardous levels. It can also remove toxins or drugs from the blood in an emergency setting.
INTRODUCTION
TYPES OF DIALYSIS:
There are different types of dialysis.
- Intermittent hemodialysis (IHD)
- Peritoneal dialysis (PD)
- Continuous renal replacement therapies (CRRT)
The choice will depend on factors such as the patient’s situation, availability, and cost.
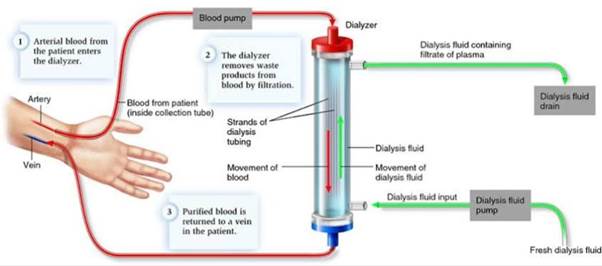
1. Intermittent hemodialysis (IHD):
IHD is highly effective in achieving solute removal by solute clearance and fluid removal by ultrafiltration. However, IHD achieves this over a short period of time, typically 3–5 hours. However, IHD induced rapid fluid removal and solute changes may result in further hemodynamic instability in critically ill patients and may result in disequilibrium syndrome in patients with pre-existing cerebral edema or severe uremia. In hemodialysis, the blood circulates outside the body. It goes through a machine with special filters. The blood comes out of the patient through a flexible tube known as a catheter. The tube is inserted into the vein. Like the kidneys, the filters remove the waste products from the blood. The filtered blood then returns to the patient through another catheter. The system works like an artificial kidney. Those who are going to have hemodialysis need surgery to enlarge a blood vessel, usually in the arm. Enlarging the vein makes it possible to insert the catheters.
During hemodialysis, your blood travels through tubes from your body into a dialysis machine. While your blood is in the machine, it goes through a filter called a dialyzer, which cleans your blood by removing some of the waste and extra fluid. Then, the cleaned blood travels through tubes from the dialysis machine back into your body. To get your blood into the dialyzer, your doctor needs to make an access, or entry into your blood vessels. This is called vascular access.
 |
Before you can begin hemodialysis, you will need minor surgery to get a vascular access. This is a way for your blood to flow in and out of your body to the dialysis machine. At the start of each hemodialysis treatment, a dialysis technician will place 2 needles in your arm using the vascular access. Your blood will flow through one needle from your vascular access to the dialysis machine, and then from the dialysis machine back to your body through the other needle. There are 3 types of vascular access:
- AV (arteriovenous) fistula: The AV fistula is the safest type of vascular access. It can last for years and is least likely to get infections or blood clots. A surgeon connects an artery (a large blood vessel that carries blood from your heart) and a vein (a blood vessel that carries blood to your heart) under the skin in your arm. Usually, they do the AV fistula in your non-dominant arm. For example, if you are right-handed, you would probably get your fistula in your left arm. Because the fistula needs time to heal after surgery, it’s best to get an AV fistula 2–3 months before you need to start dialysis. After 2-3 months, the fistula will be stronger than a normal artery or vein to allow needles to be put in and taken out many times a week.
- AV graft: An AV graft is the next best vascular access option. It’s more likely to have problems with infections and blood clots. A surgeon uses a plastic tube to connect an artery and vein under the skin in your arm. It’s best to get an AV graft 2–3 weeks before you start dialysis.
- Catheter: A catheter is a Y-shaped plastic tube. Catheters are more likely to have problems with infection, blood clots, and scarring. One end connects to a large vein that is deeper inside your body. The other two ends come out through your skin. There are 2 types of catheters, ( venous catheter and tunneled catheter ).
Procedure: - During hemodialysis, you’ll sit or lie back in a chair. A tech will place two needles in your arm where the fistula or graft is located. A pump in the hemodialysis machine slowly draws out your blood, then sends it through another machine called a dialyzer. This works like a kidney and filters out extra salt, waste, and fluid. Your cleaned blood is sent back into your body through the second needle in your arm. Or, if there’s a catheter, blood comes out of one port and then is returned via a second port.
2. Peritoneal dialysis:
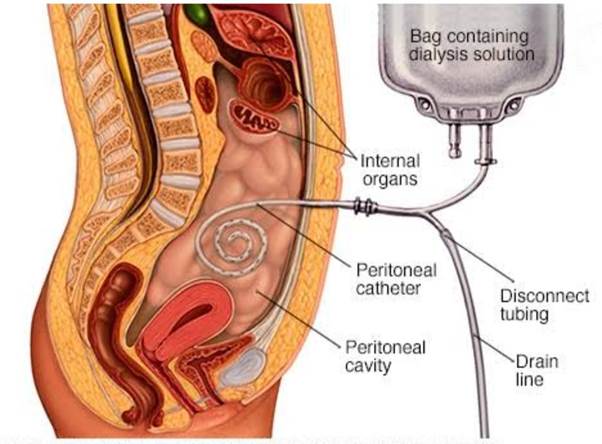
Although peritoneal dialysis is still used widely in developing countries and in neonates, often with excellent outcomes, it has limitations in efficiency of solute clearance and in patients following abdominal surgery. While hemodialysis removes impurities by filtering the blood, peritoneal dialysis works through diffusion. In peritoneal dialysis, a sterile dialysate solution, rich in minerals and glucose, is run through a tube into the peritoneal cavity, the abdominal body cavity that surrounds the intestine. It has a semi-permeable membrane, the peritoneal membrane. Peritoneal dialysis uses the natural filtering ability of the peritoneum, the internal lining of the abdomen, to filter waste products from the blood. There are two main types of peritoneal dialysis:
- Continuous ambulatory peritoneal dialysis (CAPD) requires no machinery, and the patient or a caregiver can do it. The dialysate is left in the abdomen for up to 8 hours and then replaced with a fresh solution straight away. This happens every day, four or five times per day.
- Continuous cyclic peritoneal dialysis (CCPD), or automated peritoneal dialysis uses a machine to exchange the fluids. It is generally done every night, while the patient sleeps.
Each session lasts from 10 to 12 hours. After spending the night attached to the machine, most people keep the fluid inside their abdomen during the day. Some patients may need another exchange during the day.
PD uses the thin lining of the abdomen called the peritoneum as a filter. During treatments, a cleansing fluid called dialysate is cycled into the patient’s abdomen through a small, flexible tube called a PD catheter. The dialysate absorbs or pulls extra waste and fluids from blood vessels in the abdominal lining into the peritoneal cavity where it stays in the abdomen for a specified amount of time (dwell time). The PD machine then drains the fluid out of the abdomen and into a drain or waste bag and the excess wastes and fluids are removed from the body. Then, fresh dialysate is sent back into the to peritoneum to clean the blood once more. This filling and draining process is called an exchange or cycle.
 |
Peritoneal dialysis may be done to manage kidney failure until a kidney transplant is possible. Kidney failure itself usually results from a long-term (chronic) disease that causes kidney damage over a number of years. Common causes of kidney failure include:
- Diabetes
- High blood pressure (hypertension)
- Kidney inflammation (glomerulonephritis)
- Multiple cysts in the kidneys (polycystic kidney disease)
Peritoneal dialysis may be the better option if: You can’t tolerate the rapid changes of fluid balance associated with hemodialysis. During hemodialysis, your blood is pumped into a machine to be filtered and then returned to your body. You want to minimize the disruption of your daily activities and work or travel more easily.
Peritoneal dialysis might not work for you if: You have extensive surgical scars in your abdomen. You have a large abdominal hernia. You have a limited ability to care for yourself or lack caregiving support at home. You have inflammatory bowel disease or frequent bouts of diverticulitis.
Procedure: - Before you start peritoneal dialysis, you will receive training on what the procedure involves and how to use the equipment. Plus, you'll need an operation to insert the catheter — the thin, soft plastic tube that carries the dialysis solution in and out of your abdomen. You may receive local or general anesthetics for the surgical insertion procedure. Usually the surgeon places the tube near your bellybutton. Your doctor will probably recommend waiting at least two weeks before starting treatment so that the catheter site has time to heal.
1. Continuous Ambulatory Peritoneal Dialysis (CAPD)
This 3-step process is called an exchange.
Step 1: Fill - A bag of solution called dialysate is put into the abdomen through the catheter. This bag holds about 2 quarts of fluid. It takes about 10 to 20 Minutes to fill. When the bag is empty, it can be clamped off or the tubing can be capped off.
Step 2: Dwell - The solution stays in the abdomen 4 to 6 hours. While the solution is in the abdomen, extra fluid and wastes move from the blood and into the solution.
Step 3: Drain - Using gravity, the solution is then drained out of the body into a drain bag. The drained fluid is much like urine and will be clear yellow. It takes about 10 to 20 minutes to drain.
When the solution is drained, a new bag of dialysate is connected to the catheter and the steps are repeated. These 3 steps are done about 4 times each day with meals and at bedtime. Each cycle takes 20 to 40 minutes. After you are trained, you can do peritoneal dialysis anywhere there is a clean, private area. To prevent infection, the exchange must be done under clean conditions and the patient may need to wear gloves and a mask.
2. Continuous Cycling Peritoneal Dialysis (CCPD)
With CCPD, there are fill, dwell and drain cycles, but the dwell time is shorter and a machine does the exchanges. The dwell time is about 1½ hours. The machine is set up and the person is connected to this machine for 8 to 10 hours during the night. The person is unhooked from the machine during the day.
3. Continuous renal replacement therapy:
Continuous renal replacement therapy (CRRT) provides for fluid removal and solute clearance continuously, 24 hours a day, potentially allowing for less hemodynamic instability. Some studies have shown significant hemodynamic instability in critically ill patients during IHD and even during slow low efficiency dialysis (SLED) which uses a lower blood and dialysate flow rate and extends dialysis to 8 or more hours. However, others have not, especially from centers where the initial blood pump speed is slow, the duration of IHD is extended to 5 or 6 hours and is performed daily so to minimize solute shifts and the amount of fluid removal required. There are different types of CRRT. It can involve trusted source either filtration or diffusion. It is better tolerated than intermittent dialysis, because the solute or fluid removal is slower. This leads to fewer complications, for example, a lower chance of hypotension.
CRRT is based on four main physiologic principles. These are (a) diffusion, (b) ultraflltration, (c) convection, and (d) adsorption. [5] In clinical practice, there is more than one principle implemented in achieving the goals of required treatment (e. g., diffusion, ultraflltration, and convection). CRRT can be performed in one or more of the following four modalities: (1) slow continuous ultraflltration (SCUF), (2) CVVH, (3) continuous veno-venous hemodiafiltration (CVVHDF), and (4) continuous veno-venous HD (CVVHD). Other therapeutic modalities that can be used in conjunction with CRRT include therapeutic plasma exchange and hemoperfusion/adsorption.
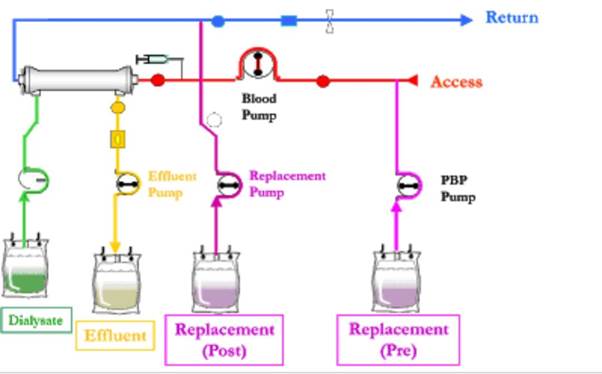
Procedure: - There are six medical products required to perform CRRT on a patient:
1. Blood purification machine: the machine pumps the blood, controls the rate of blood flow and includes software to safely monitor therapy delivery.
2. Dialysate: a fluid that carries toxins away from the filter.
3. Replacement fluid: a specialized, sterile fluid also used to flush toxins from the body but also to replace electrolytes, other blood elements and volume lost during the filtration process.
4. Filter: machine component that removes fluid and uremic toxins.
5. Anticoagulation method: a type of drug that helps the blood flow through the system, lessening the likelihood that the blood will clot in the filter.
6. Blood warmer: efficiently maintains a patient’s blood temperature during blood purification therapy.
During this therapy, a patient’s blood passes through a special filter that removes fluid and uremic toxins, returning clean blood to the body. The slow and continuous nature of the process, typically performed over a 24-hour period, allows patients with unstable blood pressure and heart rates, which is termed hemodynamically unstable, to better tolerate this process.
INDICATIONS:
1. Hemodialysis: - Indications of dialysis in acute renal failure (ARF)
- Severe fluid overload
- Refractory hypertension
- Uncontrollable hyperkalemia
- Nausea, vomiting, poor appetite, gastritis with hemorrhage
- Lethargy, malaise, somnolence, stupor, coma, delirium, asterixis, tremor, seizures
- Pericarditis (risk of hemorrhage or tamponade)
- Bleeding diathesis (epistaxis, gastrointestinal (GI) bleeding and etc. )
- Severe metabolic acidosis
- Blood urea nitrogen (BUN) > 70–100 mg/dl
Indications of dialysis in chronic renal failure (CRF)
- Pericarditis
- Fluid overload or pulmonary edema refractory to diuretics
- Accelerated hypertension poorly responsive to antihypertensives
- Progressive uremic encephalopathy or neuropathy such as confusion, asterixis, myoclonus, wrist or foot drop, seizures
- Bleeding diathesis attributable to uremia.
2. Peritoneal dialysis: - Some absolute and relative indications
Absolute indications:
- Poor cardiac function
- Peripheral vascular disease
Relative indications.
- Free life style
- % Want to take care themselves
- Long distance to hemodialysis center
✓ Uremic symptoms with neurologic abnormalities
✓ Persistent hyperkalemia, above 6. 5 mEq/L
✓ Blood urea level more than 50 mmol/l Serum Creatinine more than 900 pmol/l
✓ Severe acidosis, pH less than 7. 2,
✓ TC02 less than 10-12 mEq/L
✓ Hyperphosphatemia
✓ Pulmonary edema and CCF
3. Continuous renal replacement therapy: - Initiation of CRRT is indicated in patients with
(a) hemodynamic instability/shock
(b) diuretic-resistant fluid overload
(c) severe metabolic acidosis (pH < 7. 2), and
(d) refractory hyperkalemia (K+ > 6. 5).
CRRT has also been considered in drug toxicity and in the prevention of radiocontrast-induced nephro-pathy, though the latter has not been confirmed in a meta-analysis study. The goals of CRRT include
(i) clearance of uremic toxins
(ii) correction of electrolytes disturbance
(iii) acid-base balance
(iv) hemodynamic stabilization
(v) fluid balance,
(vi) nutritional support
(vii) removal and/or modulation of inflammatory mediators in septic patients.
CONTRAINDICATIONS:
1. Absolute contraindication to hemodialysis is the inability to secure vascular access, and relative contraindications involve difficult vascular access, needle phobia, cardiac failure, and coagulopathy. Relative contraindications like needle aversion can be overcome by careful use of local anesthetics and nursing encouragement. Severe coagulopathy complicates the maintenance of anticoagulation in the extracorporeal circuit.
2. Clinical contraindications include inflammatory abdominal processes such as Crohn disease, ulcerative colitis, current clostridium difficile infection, and end-stage liver disease with ascites. The main anatomic contraindication to PD is an unrepaired hernia that would potentially increase in size with the use of PD. Relative anatomic contraindications include the presence of ostomies or feeding tubes. Patients with a history of complex abdominal surgery with a high risk for adhesion formation would be better served with laparoscopic placement to allow for direct visualization and management of adhesions. PD is contraindicated in patients with documented Type II ultrafiltration failure, severe inflammatory bowel disease, active acute diverticulitis, abdominal abscess, active ischemic bowel disease, severe active psychotic disorder, marked intellectual disability, and in women starting dialysis in the third trimester of pregnancy. In most of the remaining situations, either HD or PD is equally preferred.
3. The main contraindication for CRRT is the need to have treatment outcomes reached more rapidly than the CRRT treatment can accomplish. In critically ill patients, who frequently have contraindications to systemic anticoagulation, regional anticoagulation with trisodium citrate is an increasingly accepted method due to its safety and efficiency if applied under strict metabolic control. Regional anticoagulation with UFH/protamin now has limited use because of side effects related to protamin. In patients with contraindication to heparinization, new drugs not yet available in Brazil, such as prostaglandins, recombinant hirudin, argatroban and nafamostat can be used.
COMPLICATIONS:
1. Hemodialysis complications: - Hypotension (Low blood pressure) - This is related to the speed and amount of fluid removed from your blood. Giving you some intravenous fluids can easily reverse this. Symptoms can vary. Tell the nurse if you experience dizziness, nausea, cramps in legs or any ‘funny feeling’. The best way to prevent this is for you to stick to the fluid restrictions that are set for you so that you avoid gaining too much fluid/weight between dialysis sessions.
Fluid Overload - Between sessions, patients can some times develop a condition called fluid overload. This is due to excess fluid building up in your body. Fluid overload can be mild and manifest itself as swollen ankles, or high blood pressure, or severe breathlessness. Constantly becoming fluid overloaded is not good for you, as it causes the blood pressure to rise and eventually damage the heart. If you think you are overloaded, contact the dialysis unit to organise extra dialysis to remove the fluid. If you are breathless or unwell, do not delay in contacting the dialysis unit.
Bleeding From Access Point - After dialysis, the needles will be removed from your fistula or graft. Your nurse will take every care to ensure that bleeding has stopped before you leave the unit. If you should develop further bleeding, from your access site, apply a dry dressing to the site, apply gentle pressure to the area, and return to the unit immediately. If possible, call the unit to let them know.
|
|
|
© helpiks.su При использовании или копировании материалов прямая ссылка на сайт обязательна.
|