
- Автоматизация
- Антропология
- Археология
- Архитектура
- Биология
- Ботаника
- Бухгалтерия
- Военная наука
- Генетика
- География
- Геология
- Демография
- Деревообработка
- Журналистика
- Зоология
- Изобретательство
- Информатика
- Искусство
- История
- Кинематография
- Компьютеризация
- Косметика
- Кулинария
- Культура
- Лексикология
- Лингвистика
- Литература
- Логика
- Маркетинг
- Математика
- Материаловедение
- Медицина
- Менеджмент
- Металлургия
- Метрология
- Механика
- Музыка
- Науковедение
- Образование
- Охрана Труда
- Педагогика
- Полиграфия
- Политология
- Право
- Предпринимательство
- Приборостроение
- Программирование
- Производство
- Промышленность
- Психология
- Радиосвязь
- Религия
- Риторика
- Социология
- Спорт
- Стандартизация
- Статистика
- Строительство
- Технологии
- Торговля
- Транспорт
- Фармакология
- Физика
- Физиология
- Философия
- Финансы
- Химия
- Хозяйство
- Черчение
- Экология
- Экономика
- Электроника
- Электротехника
- Энергетика
Poor Gas Exchange. Blood carries oxygen to cells throughout your body and carbon dioxide away from them. But because you're not breathing in and out fully, you may have less oxygen than you need or more carbon dioxide than you should in your blood. Eithe
Poor Gas Exchange
Blood carries oxygen to cells throughout your body and carbon dioxide away from them. But because you're not breathing in and out fully, you may have less oxygen than you need or more carbon dioxide than you should in your blood. Either of these may be why you have shortness of breath. A high carbon dioxide level can also give you a headache and make you woozy. A simple device called an oximeter that goes on your fingertip can check your oxygen level. Extra oxygen should help get that level up to where your doctor recommends. But if you're using oxygen, keep the flow within the range your doctor prescribed. Sometimes, too much oxygen can cause serious problems.
Heart Problems
Low blood oxygen levels can lead to narrowed arteries and higher blood pressure in the blood vessels that go from your heart to your lungs, as well as within your lungs. That can put a lot of stress on your heart, making it work harder than it should. It could become heart failure, a permanent condition in which your heart is too weak to do its job well.
Atrial Fibrillation
COPD can damage nerve fibers that connect to the heart and cause unusual heartbeats called arrhythmia. Atrial fibrillation (AFib) is the most common arrhythmia. In a study of more than 1. 3 million people with COPD, about 18% also had AFib.
Thinning Bones (Osteoporosis)
It's common for people with COPD to get osteoporosis. They've often been smokers, they take steroids, it's hard for them to get enough bone-strengthening exercise, and they can be low on bone-building vitamin D.
Weak Arms and Legs
Some of the same things that cause bone loss can cause muscle loss, too. Those weak muscles make it even harder to do everyday activities. Ask your doctor to check how well your limbs work. A pulmonary rehab program can help preserve muscle. It may include strength training to build up muscle tissue you've lost.
Weight Issues
When you're overweight, your lungs have to work harder. This can make your COPD worse and complications more likely.
Sleep Problems
COPD symptoms can wake you up during the night, which will leave you tired during the day. Even more serious is sleep apnea, a condition in which you have repeated pauses in breathing while you sleep. The pauses, along with low oxygen levels, could make your COPD worse.
Diabetes
Many people with COPD have diabetes. The damage caused by one can make the other more likely. Exercise and quitting smoking help with both conditions. Also make sure that all of your doctors know what the others have prescribed.
Depression and Anxiety
At least 1 in 10 people with early COPD get depression or anxiety, and that number climbs as the disease gets worse. Medication can help, along with exercise and even music therapy. Work with your doctor or a therapist on self-care skills, too. People who problem-solve do better physically and emotionally than people who ignore health issues.
Lung Cancer
You’re more likely to get lung cancer if you have COPD. And when you do get it, the outcome after diagnosis and treatment tends to be worse than someone without COPD. Some scientists think the two disease are different aspects of the same condition. Others think that COPD is a driving factor that simply raises your risk for lung cancer.
Secondary Polycythemia
The “polycythemia” means that the number of red blood cells has increased. The “secondary” means that it is the result of an underlying condition like sleep apnea, obesity hypoventilation syndrome, and COPD. COPD lessens oxygen, which can raise levels of erythropoietin and lead to secondary polycythemia. You might have a headache and feel tired, sluggish, or confused. It also raises your risk for strokeProper treatment of the underlying condition -- in this case COPD -- can help control secondary polycythemia.
Types of COPD
COPD is an umbrella term used when you have one or more of these conditions: Emphysema. This results from damage to your lungs’ air sacs (alveoli) that destroys the walls inside them and causes them to merge into one giant air sac. It can’t absorb oxygen as well, so you get less oxygen in your blood. Damaged alveoli can make your lungs stretch out and lose their springiness. Air gets trapped in your lungs and you can’t breathe it out, so you feel short of breath.
Chronic bronchitis. If you have coughing, shortness of breath, and mucus that lingers at least 3 months for 2 years in a row, you have chronic bronchitis. Hair-like fibers called cilia line your bronchial tubes and help move mucus out. When you have chronic bronchitis, you lose your cilia. This makes it harder to get rid of mucus, which makes you cough more, which creates more mucus.
Emphysema
Emphysema is a disease of the lungs that usually develops after many years of smoking. Along with asthma and chronic bronchitis, emphysema belongs to a group of lung diseases known as chronic obstructive pulmonary disease (COPD).
Emphysema is a disease of the lungs that usually develops after many years of smoking. Both chronic bronchitis and emphysema belong to a group of lung diseases known as chronic obstructive pulmonary disease (COPD). Once it develops, emphysema can’t be reversed. This is why not smoking or stopping smoking is very important.
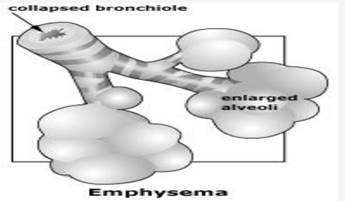
Emphysema is a condition that involves damage to the walls of the air sacs (alveoli) of the lung. Alveoli are small, thin-walled, very fragile air sacs located in clusters at the end of the bronchial tubes deep inside the lungs. There are about 300 million alveoli in normal lungs. As you breathe in air, the alveoli stretch, drawing oxygen in and transporting it to the blood. When you exhale, the alveoli shrink, forcing carbon dioxide out of the body.
When emphysema develops, the alveoli and lung tissue are destroyed. With this damage, the alveoli cannot support the bronchial tubes. The tubes collapse and cause an “obstruction” (a blockage), which traps air inside the lungs. Too much air trapped in the lungs can give some patients a barrel-chested appearance. Also, because there are fewer alveoli, less oxygen will be able to move into the bloodstream.
Smoking is the number one factor. Because of this, emphysema is one of the most preventable types of respiratory diseases. Air pollutants in the home and workplace, genetic (inherited) factors (alpha-1 antitrypsin deficiency), and respiratory infections can also play a role in causing emphysema.
Cigarette smoking not only destroys lung tissue, it also irritates the airways. This causes inflammation and damage to cilia that line the bronchial tubes. This results in swollen airways, mucus production, and difficulty clearing the airways. All of these changes can lead to shortness of breath.
Symptoms of emphysema may include coughing, wheezing, shortness of breath, chest tightness, and an increased production of mucus. Often times, symptoms may not be noticed until 50 percent or more of the lung tissue has been destroyed. Until then, the only symptoms may be a gradual development of shortness of breath and tiredness (fatigue), which can be mistaken for other illnesses. People who develop emphysema have an increased risk of pneumonia, bronchitis, and other lung infections. See your doctor if any of these symptoms arise:
Shortness of breath, especially during light exercise or climbing steps
Ongoing feeling of not being able to get enough air
Long-term cough or “smoker’s cough”
Wheezing
Long-term mucus production
Ongoing fatigue
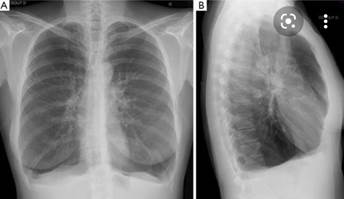
The diagnosis of emphysema cannot be made solely on symptoms. Several tests are used to make the diagnosis. One simple test is to tap on your chest and listen with a stethoscope for a hollow sound. This means that air is being trapped in your lungs. Other tests include:
X-rays: X-rays are generally not useful for detecting early stages of emphysema. However,
X-rays can help diagnose moderate or severe cases. Either a plain chest X-ray or a CAT (computer-aided tomography) scan can be used. Once the test is completed, the readings are compared to X-rays of healthy or normal lungs.
Pulse oximetry: This test is also known as an oxygen saturation test. Pulse oximetry is used to measure the oxygen content of the blood. This is done by attaching the monitor to a person’s finger, forehead, or earlobe.
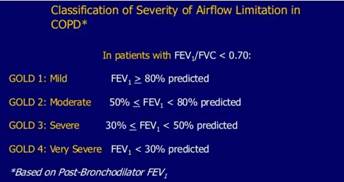
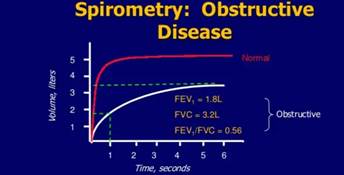
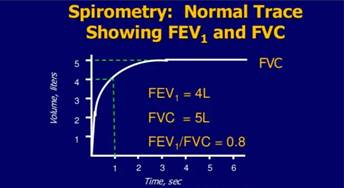
Spirometry and pulmonary function tests (PFT): This is one of the most useful tests to determine airway blockage. A spirometry or PFT tests the lungs’ volume by measuring airflow while a patient inhales and exhales. This test is done by taking a deep breath and then blowing into a tube that is hooked up to a specialized machine. These tests are compared to normal results from people of similar gender, age, height, weight and ethnic background.
Arterial blood gas: This test measures the amount of oxygen and carbon dioxide in blood from an artery. It is a test often used as emphysema worsens. It is especially helpful in determining if a patient needs extra oxygen.
Electrocardiogram (ECG): ECGs check heart function and are used to rule out heart disease as a cause of shortness of breath.
Because emphysema can worsen over time and there is no known cure, treatment is focused on slowing the speed of decline. The type of treatment will depend on the severity of the disease.
Quitting smoking: If you smoke, quit. This is the most important step you can take to protect your lungs. It is never too late to quit. Your doctor can help you find the best smoking quitting method for you.
Bronchodilator medications: These medicines relax the muscles around the airways. They are often used to treat asthma. Bronchodilators, given through hand-held inhalants, produce more immediate results and have fewer side effects than oral medications.
Anti-inflammatory medication: These medications reduce inflammation in the airways. However, long-term side effects of these drugs include osteoporosis, hypertension, high blood sugar, and fat redistribution.
Oxygen therapy: Oxygen therapy is prescribed for patients whose lungs are not getting enough oxygen to the blood (hypoxemia). These patients can’t absorb enough oxygen from the outside air and need to get more oxygen through a machine (a nasal catheter or a facemask).
Lung volume reduction surgery: Lung volume reduction surgery involves removing a portion of diseased lung tissue, then joining together the remaining tissue. Doing this may relieve pressure on the breathing muscles and help improve lung elasticity (or stretch). The results of the surgery have been very promising. Not all patients with emphysema are candidates for this surgery.
The best way to prevent or reduce further problems is to prevent respiratory infections by:
Practicing good handwashing methods
Brushing and flossing teeth daily, and using an antibacterial mouth rinse after meals
Keeping breathing equipment clean
Keeping your house clean and free of dust
Getting a flu shot every year
Following a doctor-prescribed exercise program
Avoiding irritants such as:
Cigarette smoke
Exhaust fumes
Strong perfumes
Cleaning products
Paint/varnish
Dust
Pollen
Pet dander
Pollution
Xray reports of emphysema

Chronic bronchitis
Chronic bronchitis is a type of COPD (chronic obstructive pulmonary disease). COPD is a group of lung diseases that make it hard to breathe and get worse over time. The other main type of COPD is emphysema. Most people with COPD have both emphysema and chronic bronchitis, but how severe each type is can be different from person to person.
Chronic bronchitis is inflammation (swelling) and irritation of the bronchial tubes. These tubes are the airways that carry air to and from the air sacs in your lungs. The irritation of the tubes causes mucus to build up. This mucus and the swelling of the tubes make it harder for your lungs to move oxygen in and carbon dioxide out of your body.
What causes chronic bronchitis?
The cause of chronic bronchitis is usually long-term exposure to irritants that damage your lungs and airways. In the United States, cigarette smoke is the main cause. Pipe, cigar, and other types of tobacco smoke can also cause chronic bronchitis, especially if you inhale them.
Exposure to other inhaled irritants can contribute to chronic bronchitis. These include secondhand smoke, air pollution, and chemical fumes or dusts from the environment or workplace.
Rarely, a genetic condition called alpha-1 antitrypsin deficiency can play a role in causing chronic bronchitis.
Who is at risk for chronic bronchitis?
The risk factors for chronic bronchitis include
Smoking. This the main risk factor. Up to 75% of people who have chronic bronchitis smoke or used to smoke.
Long-term exposure to other lung irritants, such as secondhand smoke, air pollution, and chemical fumes and dusts from the environment or workplace.
Age. Most people who have chronic bronchitis are at least 40 years old when their symptoms begin.
Genetics. This includes alpha-1 antitrypsin deficiency, which is a genetic condition. Also, smokers who get chronic bronchitis are more likely to get it if they have a family history of COPD.
What are the symptoms of chronic bronchitis?
At first, you may have no symptoms or only mild symptoms. As the disease gets worse, your symptoms usually become more severe. They can include
Frequent coughing or a cough that produces a lot mucus
Wheezing
A whistling or squeaky sound when you breathe
Shortness of breath, especially with physical activity
Tightness in your chest
Some people with chronic bronchitis get frequent respiratory infections such as colds and the flu. In severe cases, chronic bronchitis can cause weight loss, weakness in your lower muscles, and swelling in your ankles, feet, or legs.
There is no cure for chronic bronchitis. However, treatments can help with symptoms, slow the progress of the disease, and improve your ability to stay active. There are also treatments to prevent or treat complications of the disease. Treatments include
Lifestyle changes, such as
Quitting smoking if you are a smoker. This is the most important step you can take to treat chronic bronchitis.
Avoiding secondhand smoke and places where you might breathe in other lung irritants
Ask your health care provider for an eating plan that will meet your nutritional needs. Also ask about how much physical activity you can do. Physical activity can strengthen the muscles that help you breathe and improve your overall wellness.
Medicines, such as
Bronchodilators, which relax the muscles around your airways. This helps open your airways and makes breathing easier. Most bronchodilators are taken through an inhaler. In more severe cases, the inhaler may also contain steroids to reduce inflammation.
Vaccines for the flu and pneumococcal pneumonia, since people with chronic bronchitis are at higher risk for serious problems from these diseases.
Antibiotics if you get a bacterial or viral lung infection
Oxygen therapy, if you have severe chronic bronchitis and low levels of oxygen in your blood. Oxygen therapy can help you breathe better. You may need extra oxygen all the time or only at certain times.
Pulmonary rehabilitation, which is a program that helps improve the well-being of people who have chronic breathing problems. It may include
An exercise program
Disease management training
Nutritional counseling
Psychological counseling
A lung transplant, as a last resort for people who have severe symptoms that have not gotten better with medicines
If you have chronic bronchitis, it's important to know when and where to get help for your symptoms. You should get emergency care if you have severe symptoms, such as trouble catching your breath or talking. Call your health care provider if your symptoms are getting worse or if you have signs of an infection, such as a fever.
Can chronic bronchitis be prevented?
Since smoking causes most cases of chronic bronchitis, the best way to prevent it is to not smoke. It's also important to try to avoid lung irritants such as secondhand smoke, air pollution, chemical fumes, and dusts.
Chronic bronchitis occurs when the lining of the bronchial tubes repeatedly becomes irritated and inflamed. The continuous irritation and swelling can damage the airways and cause a buildup of sticky mucus, making it difficult for air to move through the lungs. This leads to breathing difficulties that gradually get worse. The inflammation can also damage the cilia, which are the hair-like structures that help to keep the air passages free of germs and other irritants. When the cilia don’t work properly, the airways often become a breeding ground for bacterial and viral infections.
Infections typically trigger the initial irritation and swelling that lead to acute bronchitis. Chronic bronchitis, however, is most commonly caused by cigarette smoking. In fact, over 90 percent of those with the disease have a history of smoking. Inhaling cigarette smoke temporarily paralyzes the cilia, so frequent smoking over an extended period can severely damage the cilia. Chronic bronchitis may develop over time due to this damage.
Secondhand smoke can also contribute to the development of chronic bronchitis. Other possible causes include extended exposure to air pollution, industrial or chemical fumes, and toxic gases. Repeated lung infections may also cause further damage to the lungs and make chronic bronchitis symptoms worse.
Depending on the severity of your condition, your treatment plan may consist of the following:
A bronchodilator is a type of medicine that opens the airways in your lungs, making it easier to breathe. The substance is usually breathed in through an inhaler, which is a device that pumps the medicine into your lungs. Your doctor will show you how to use your inhaler properly so you get the most from bronchodilator.
Theophylline is an oral medication that relaxes the muscles in your airways so they open up more, which helps relieve any breathing difficulties. Your doctor may prescribe theophylline if you have severe shortness of breath.
If your symptoms don’t improve with bronchodilator or theophylline, your doctor might prescribe steroids. These medications can be taken either with an inhaler or in pill form.
Pulmonary rehabilitation is a program that is meant to improve your breathing and overall well-being. It often consists of exercise, nutritional counseling, and breathing strategies. Some programs also include counseling. Your doctor may refer you to a pulmonary rehabilitation program at a hospital in your area.
Lifestyle Remedies
Making certain lifestyle changes and trying natural remedies can also help alleviate the symptoms of chronic bronchitis. You may want to consider the following:
Breathing in warm, moist air from a humidifier can ease coughs and loosen the mucus in your airways. Make sure you clean the humidifier regularly according to the manufacturer’s instructions. Bacteria and fungi can grow in the water container if it isn’t cleaned properly.
You should quit smoking immediately if you’re smoker. If you live in an area with high levels of air pollution, you should wear a mask whenever you go outside. You should also wear a mask if you work in an industry where you’re exposed to paint or household cleaners with strong fumes. Frequent exposure to these irritants can make your symptoms much worse.
Physical activity can strengthen the muscles that help you breathe. Ideally, you should exercise at least three times per week for 30 minutes. If you didn’t work out before, start out slowly and gradually increase the length and intensity of your exercise routine. You can ask your doctor to help you create an exercise plan that works for you.
Pursed-lip breathing can sometimes provide relief when you’re having difficulty breathing. In pursed-lip breathing, you take a deep breath and then slowly breathe out through your mouth. As you breathe out, hold your lips as if you’re about to kiss someone. Doing this can help regulate your breathing and make you feel better when you’re experiencing shortness of breath.
X-ray images


There is no cure for chronic bronchitis. However, treatments can help with symptoms, slow the progress of the disease, and improve your ability to stay active. There are also treatments to prevent or treat complications of the disease. Treatments include
Lifestyle changes, such as
Quitting smoking if you are a smoker. This is the most important step you can take to treat chronic bronchitis.
Avoiding secondhand smoke and places where you might breathe in other lung irritants
Ask your health care provider for an eating plan that will meet your nutritional needs. Also ask about how much physical activity you can do. Physical activity can strengthen the muscles that help you breathe and improve your overall wellness.
Medicines, such as
Bronchodilators, which relax the muscles around your airways. This helps open your airways and makes breathing easier. Most bronchodilators are taken through an inhaler. In more severe cases, the inhaler may also contain steroids to reduce inflammation.
Vaccines for the flu and pneumococcal pneumonia, since people with chronic bronchitis are at higher risk for serious problems from these diseases.
Antibiotics if you get a bacterial or viral lung infection
Oxygen therapy, if you have severe chronic bronchitis and low levels of oxygen in your blood. Oxygen therapy can help you breathe better. You may need extra oxygen all the time or only at certain times.
Pulmonary rehabilitation, which is a program that helps improve the well-being of people who have chronic breathing problems. It may include
An exercise program
Disease management training
Nutritional counseling
Psychological counseling
A lung transplant, as a last resort for people who have severe symptoms that have not gotten better with medicines
If you have chronic bronchitis, it's important to know when and where to get help for your symptoms. You should get emergency care if you have severe symptoms, such as trouble catching your breath or talking. Call your health care provider if your symptoms are getting worse or if you have signs of an infection, such as a fever.
Since smoking causes most cases of chronic bronchitis, the best way to prevent it is to not smoke. It's also important to try to avoid lung irritants such as secondhand smoke, air pollution, chemical fumes, and dusts
Since smoking causes most cases of chronic bronchitis, the best way to prevent it is to not smoke. It's also important to try to avoid lung irritants such as secondhand smoke, air pollution, chemical fumes, and dusts
Conclusion: -
In conclusion, COPD is a global disease, with increasing prevalence and health-related impact. The loss of FEV1 may be slowing down, but what is really needed is an intervention that improves it in the long-term. It is important to identify patients with the frequent-exacerbation phenotype using clinical predictors such as chronic bronchitis, GERD and history of previous exacerbations. Performing a CT scan should not be done routinely, but can be useful in patients with severe disease. The findings may include bronchiectasis or an enlarged pulmonary artery, both clinically useful in identifying those at risk of recurrent exacerbations. COPD exacerbations are a major cause of mortality and morbidity, and it is important to recognize that they are inflammatory events primarily driven by infections, so antibiotic treatment according to a stratified approach is the right way to go as they are helpful in eradicating the bacteria and reducing the relapse rate. COPD is preventable, something that was always known, but physicians have to change our attitude in treating this disease.
Relief of symptoms, reduction of exacerbations and improvement in quality of life should be our primary aim when approaching COPD patients. Out of the pipelines, tremendous ongoing research is being done to obtain new bronchodilators and anti-inflammatory therapies for COPD, with a lot of focus and promise in finding the magic bullet for this chronic and debilitating disease.
Page-11
REFERENCE: -
.
American Thoracic Society, European Respiratory Society. Standards for the Diagnosis and Management of Patients with COPD. 2004. PMID: None.
2.
Celli BR, Macnee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004 Jun; 23(6): 932–46. [PubMed]
3.
National Institute for Health and Clinical Excellence. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care. 2010. PMID: None. [PubMed]
4.
Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011 Aug 2; 155(3): 179–91. [PubMed]
5.
Wilt TJ, Niewoehner D, MacDonald R, et al. Management of stable chronic obstructive pulmonary disease: a systematic review for a clinical practice guideline. Ann Intern Med. 2007 Nov 6; 147(9): 639–53. [PubMed]
6.
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2015. PMID: None. [PubMed]
7.
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005 Nov; 26(5): 948–68. [PubMed]
8.
Cerveri I, Corsico AG, Accordini S, et al. Underestimation of airflow obstruction among young adults using FEV1/FVC < 70% as a fixed cut-off: a longitudinal evaluation of clinical and functional outcomes. Thorax. 2008 Dec; 63(12): 1040–5. [PubMed]
9.
van Dijk WD, Gupta N, Tan WC, et al. Clinical Relevance of Diagnosing COPD by Fixed Ratio or Lower Limit of Normal: A Systematic Review. COPD. 2013 Jul 17 [PubMed]
10.
Runarsdottir SB, Gudmundsson G, Aspelund T, et al. Prevalence of airflow obstruction in nonsmoking older individuals using different spirometric criteria: the AGES Reykjavik Study. Copd: Journal of Chronic Obstructive Pulmonary Disease. 2013 Aug; 10(4): 493–9. [PMC free article] [PubMed]
|
|
|
© helpiks.su При использовании или копировании материалов прямая ссылка на сайт обязательна.
|