
- Автоматизация
- Антропология
- Археология
- Архитектура
- Биология
- Ботаника
- Бухгалтерия
- Военная наука
- Генетика
- География
- Геология
- Демография
- Деревообработка
- Журналистика
- Зоология
- Изобретательство
- Информатика
- Искусство
- История
- Кинематография
- Компьютеризация
- Косметика
- Кулинария
- Культура
- Лексикология
- Лингвистика
- Литература
- Логика
- Маркетинг
- Математика
- Материаловедение
- Медицина
- Менеджмент
- Металлургия
- Метрология
- Механика
- Музыка
- Науковедение
- Образование
- Охрана Труда
- Педагогика
- Полиграфия
- Политология
- Право
- Предпринимательство
- Приборостроение
- Программирование
- Производство
- Промышленность
- Психология
- Радиосвязь
- Религия
- Риторика
- Социология
- Спорт
- Стандартизация
- Статистика
- Строительство
- Технологии
- Торговля
- Транспорт
- Фармакология
- Физика
- Физиология
- Философия
- Финансы
- Химия
- Хозяйство
- Черчение
- Экология
- Экономика
- Электроника
- Электротехника
- Энергетика
Treatment
MINISTRY OF EDUCATION AND SCIENCE OF RUSSIAN FEDERATION
Federal State Autonomous Educational Institution of Higher Education
«V. I. VERNADSKY CRIMEAN FEDERAL UNIVERSITY»
Medical Academy named after S. I. Georgievsky (structural subdivision).
ABSTRACT
SUBJECT: - CLINICAL COURSE AND TREATMENT OF GLOMERULONEPHRITIS DEPENDING ON MORPHOLOGICAL TYPES
STUDENT : - ABHISHEK DUBEY
faculty : - hospital practice Course : - 3RD year Group : - 182 (2) LA -1
NAME OF PRACTICE: - PHYSICAL ASSISTANT IN IN -PATIENT MEDICAL DEPARTMENT
Simferopol 2021
Page-1
INTRODUCTION: -
The term glomerulonephritis encompasses a range of immunemediated disorders that cause inflammation within the glomerulus and other compartments of the kidney. Studies with animal models have shown the crucial interaction between bonemarrow-derived inflammatory cells and cells intrinsic to the kidney that is both fundamental and unique to the pathogenesis of glomerulonephritis. The mechanisms of interaction between these cells and the mediators of their coordinated response to inflammation are being elucidated. Despite these pathophysiological advances, treatments for glomerulonephritis remain non-specific, hazardous, and only partly successful. Glomerulonephritis therefore remains a common cause of endstage kidney failure worldwide. Molecule-specific approaches offer hope for more effective and safer treatments in the future. The differential diagnosis of glomerulonephritis without systemic disease includes poststreptococcal glomerulonephritis, IgA nephropathy, rapidly progressive glomerulonephritis (RPGN), and membranoproliferative glomerulonephritis (MPGN). Glomerular inflammation is probably induced directly by a nephritogenic streptococcal protein in poststreptococcal glomerulonephritis, and by mesangial deposition of abnormally glycosylated IgA1containing immune aggregates in IgA nephropathy. In crescentic RPGN the role of cellular rather than humoral immune mechanisms is now becoming clear. Many patients with MPGN have chronic hepatitis C infection. There is no effective diseasespecific therapy for poststreptococcal glomerulonephritis or IgA nephropathy. RPGN benefits from high-dose steroids and cytotoxic drug therapy with the addition of plasma exchange in
disease induced by antibody to glomerular basement membrane
. Antiviral therapies reduce the severity of MPGN due to hepatitis C virus. However, various new therapies directed at specific cytokines, growth factors, fibrin deposition, and other mediators of injury are being developed, as well as more specific and less toxic forms of immunotherapy.
Glomerulonephritis is an important cause of renal failure thought to be caused by autoimmune damage to the kidney. While each type of glomerulonephritis begins with a unique initiating stimulus, subsequent common inflammatory and fibrotic events lead to a final pathway of progressive renal damage. In this article the different forms of inflammatory glomerulonephritis and their diagnosis are discussed. In a review of therapy both immediate life saving treatment given when glomerulonephritis causes acute renal failure and more specific treatments designed to modify the underlying mechanisms of renal injury are considered.
Acute glomerulonephritis accounted for 30% of renal diagnoses, while nephrotic syndrome accounted for 28% and HenochSchö nlein purpura nephritis accounted for 16% of renal disease. Mortality in children with renal disease was 0. 4% (two of 505). All children with acute glomerulonephritis recovered or improved at last follow-up, regardless of the relationship to a streptococcal infection. In children with uncomplicated nephrotic syndrome, 91% had a complete or partial response to corticosteroids. Nephritis developed in 81 of 278 patients with Henoch-Schö nlein purpura (29%). Since 1956, a dramatic decrease in the diagnosis of acute glomerulonephritis has occurred at this pediatric hospital.
Page-2
Main part: -
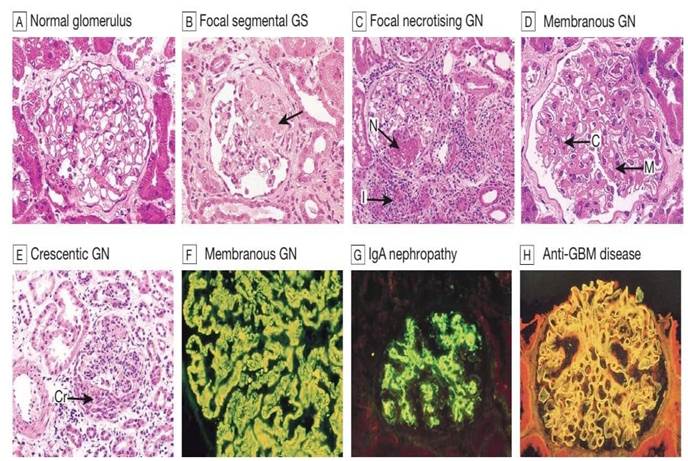
Glomerulonephritis, enabled us to divide the different forms of diffuse glomerulonephritis into 3 distinct groups and to separate these groups from the focal glomerulonephritides. The different forms of diffuse glomerulonephritis in group I are:
1. endocapillary (acute) glomeruloenphritis (of the poststreptococcal type),
2. mesangioproliferative glomerulonephritis,
3. mesangioproliferative glomerulonephritis with focal crescents,
4. mesangioproliferative glomerulonephritis with focal scarring, 5. minimal proliferating intercapillary glomerulonephritis without nephrotic syndrome. It is emphasised that these forms can transform into one another, that they seldom occur with nephrotic syndrome, and with varying frequency with hypertension. Group II consists of:
1. minimal proliferating intercapillary glomerulonephritis with nephrotic syndrome,
2. focal sclerosing glomerulonephritis,
3. perimembranous glomerulonephritis,
4. membranoproliferative glomerulonephritis,
5. lobular glomerulonephritis. It is stressed that these glomerulonephritis forms usually do not develop out of group I type glomerulonephritis forms, and that in this group a nephrotic syndrome is the most prominent clinical syndrome. In the third group are 1. mesangioproliferative glomerulonephritis with diffuse crescents,
2. necrotising glomerulonephritis. It is shown that this form of
glomerulonephritis does not usually develop from either group I of II forms.
The fourth group of focal glomerulonephritis is uncommon. This disease is characterized by a necrotising and proliferative inflammatory lesion found segmentally and focally in the glomeruli. Most of the other glomeruli appearing normal. It is emphasised that in the literature the diagnosis focal glomerulonephritis is made far too often.
This is because glomeruli in which the inflammatory process in a few lobules is of varying prominence, are included in the focal glomerulonephritis group. The classification of the different forms of glomerulonephritis into 3 groups here described, is thought of as a basic classification.
Page -3
1)Acute endocapillary diffuse proliferative glomerulonephritis
(sometimes called postinfectious or poststreptococcal glomerulonephritis) Definition:
Acute endocapillary diffuse proliferative glomerulonephritis is the
disease, which is a result of infection, leading to immuneinflammatory glomeruli affection with proliferative and exccudative changes. In some definitions the role of nephritogenic strain of group A
(β -hemolytic)
streptococci, especially type 12 is underlined. However, nowadays other types of bacterial and viral infections were found to cause the same disease.
Clinical manifestations (4 main syndromes are marked)
Page-4 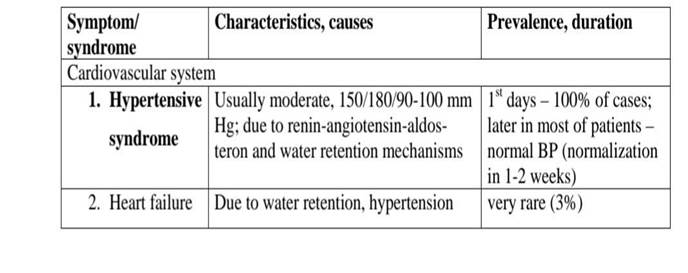
Treatment
1. Hospitalization: absolutely indicated (even in case of suspected diagnosis)
2. Strict regimen: lying in bed only for 1-2 weeks (not walking); lying
improves intrarenal haemodynamic (position leads to increase of renal blood
flow; remaining in bed leads to constant warming of the back region). Such
regimen must be kept up to 1-2 weeks or up to the period of BP
normalization, disappearance of oedemas and 10-times reduction of proteinuria and erythrocyturia. 3. Diet
A. Full complex of symptoms or nephrotic syndrome:
- 1-2 days of strict fasting: nothing should be eaten; volume of consumed water shouldn’t be more than daily diuresis.
- 2-3 days: rise and potatoes (rich by potassium): eating 4-5 times a day; each
time 200 g of milk rise porridge or 200 g of potatoes. Severe restriction of salt. Volume of fluids don’t exceed daily diuresis +500 ml - One apple day may be administered if that diet is not tolerated: 1. 5 kg of apples with reduction of water volume.
- Since 4-6 days: Protein: 40 g/24; Carbohydrates: 280-320 g; fats – 80-120 g;
Potassium – 50-60 mmol/l, Calcium 400 mg daily, Sodium 30-40 mmol/l.
Total calorage – 2500-3000 kkal; total salt – 4-5 g daily.
- This diet (severe protein and salt restriction) should be kept no less than 6
month. Milk and milk products also should be restricted due to high phosphate and proteins’ amount.
B. Isolated urinary syndrome – without fasting; from the 1st days – restriction of proteins and salt.
4. Drugs:
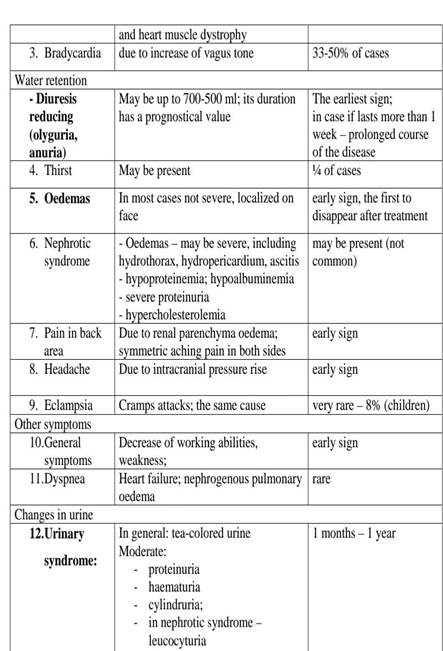 |
A. symptomatic:
|
|
|
© helpiks.su При использовании или копировании материалов прямая ссылка на сайт обязательна.
|